Before approaching an critically ill patient’s bedside you should know who the patient is and why they are in the ICU. The purpose of the history is to lay out the known facts about the patient. Usually the patient in the ICU is unable to give a clear and reliable history. You need to comb through the patient’s chart to locate this information. Dig deep! Events that may have happened months ago may have an impact on the patient today. Don’t forget, you are not the only professional that is treating the patient: ask the nurse – they are excellent historians as they give and receive a concise report at the beginning and end of each shift. It is also worth talking to the primary team, physiotherapist, pharmacist and dietician about the patient. Remember, you are one member of a team: the others may have more knowledge of the patient than you. Nevertheless you need to remain a little bit skeptical about the story that you have been given: make sure the facts match the narrative
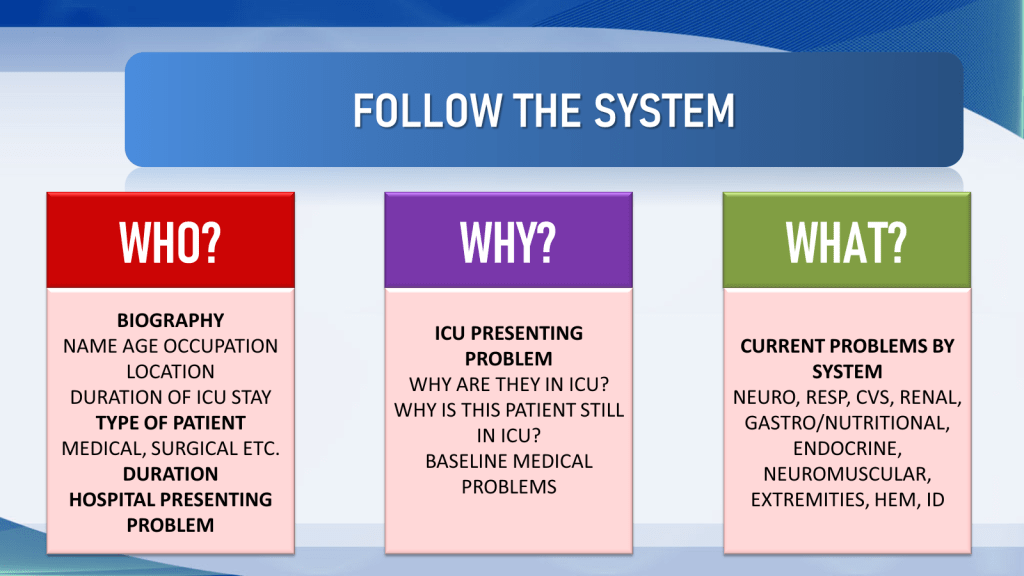
In this tutorial I will introduce the 4 Ws of clinical history: Who is this patient? Why are they in hospital and ICU. 3. What is going on with the patient (PROBLEM LIST). 4. Where are we going (what are the physiologic goals and organ based plans?).

WHO?
Who is this patient? How old are they? Where do they come from and what is their occupation?
How long has this patient been in the ICU – is this a recent admission (the patient is acutely critically ill and likely still being resuscitated)? Has the patient been in the ICU for more than 7 days? In that case the patient may be slow to recover or chronically critically ill.
What type of patient are we dealing with? Surgical or Medical? Postoperative or Critically Ill?
There are three types of critically ill patients: 1. Medical patients with an acute medical syndrome that may have occurred in the setting of low physiologic reserve. These may be children or adults. 2. Surgical patients – who have had complex elective surgery (e.g. cardiac or neurosurgery), emergency surgery or trauma. The patient may have originated as a surgical patient but now has medical problems (e.g. hospital acquired pneumonia). 3. Obstetric patients who may be currently pregnant, recently pregnant and be in ICU as a consequence of pregnancy (pre-eclampsia, post partum hemorrhage) or co-incidental with pregnancy (trauma, bowel obstruction etc.).
WHY?
It is absolutely CRITICAL that you understand the dynamics around the patient’s ICU admission. The patient may have come directly from the emergency room or operating room to ICU, or may have been transferred from a ward or other hospital. In the latter case you will need to ensure that you know exactly what went on there. These are the questions that you must ask, up front about the patient.
Why was the patient admitted to hospital?
Why was the patient admitted to ICU?
What happened in between?
What was the patient’s admission problem (MAJOR ADMISSION PROBLEM)?
This is the patient’s presenting problem (although it may not be the patient’s main current problem). It is the symptoms and diagnosis that led the patient to come into the hospital originally – e.g. chest pain, shortness of breath, confusion. This may be clarified as “pneumonia” “septic shock” etc.
Between the patient arriving in the hospital and being admitted to ICU clinical episodes may have occurred – you need to know these. Was there a delay with the diagnosis? Was a wrong pathway chosen? Did the patient deteriorate or have a cardiac or respiratory arrest on the ward?
What was the patient’s indication for ICU ADMISSION
This is a remarkably limited list because patients are admitted to ICU for life sustaining therapy consequent of single or multi organ failure. Those injuries can be summarized as follows:
- Neurological – Low GCS, Seizures
- Cardiovascular – Hypotension, Arrhythmias, Blood Loss
- Respiratory – Hypoxemia, Hypercarbia, Airway Obstruction
- Renal – AKI, Hyperkalemia, Acidosis, Dys-Osmolality, Fluid Overload
Some patients, for example those with septic shock, may have multiple system problems: confusion, hypotension, hypoxemia, oliguria – AKI.
What complications followed?
Prolonged admission to intensive care is characterized by “second and third hits” – organ injuries such as hospital acquired pneumonia, line sepsis, myocardial ischemia, acute kidney injury, bed sores etc. It is important that you are aware of these problems even if they have now resolved, as complete recovery of organ function at this stage is unlikely, and those organs remain vulnerable (for example, it is important that you do not prescribe non steroidal anti inflammatory agents (NSAIDS) to a patient who has recently recovered from acute renal failure).
What is the patient’s age and baseline health status (BACKGROUND)?
What background medical problems does the patient have? We know that patients with major organ dysfunction (such COPD, pulmonary fibrosis, heart failure (EF<40%), chronic kidney disease, cirrhosis or chronic hepatitis, previous myocardial infarction or active ischemia, connective tissue disease, inflammatory bowel disease, cancer, cerebrovascular disease, carotid arterial disease) have diminished physiologic reserve, and have a worse prognosis when admitted to intensive care. The greatest determinant of outcome, however, is the patient’s age: young patients do better in intensive care than older ones. You also need to know what medications the patient was taking pre-admission: antihypertensives, statins, SGL2 inhibitors, GLP-1 receptor agonists etc. If the patient is taking anti-coagulants you need to know why? Pulmonary embolism, stroke, atrial fibrillation, arterial obstruction, heart valve etc. All of this is relevant.
WHAT?
What PROBLEMS are keeping this patient in intensive care (CURRENT PROBLEMS)?
The patient may remain in ICU for a problem wholly unrelated to the original presenting complaint – failure to liberate from mechanical ventilation, failure to emerge from sedation etc). This is the patient’s main current problem, and it needs to be addressed. In addition, it is important to enumerate the other problems, even if they are apparently trivial.
If you don’t have a precise diagnosis don’t invent one – just list the problems, these can be padded out later
So a patient may be admitted with
Hypoxic Respiratory Failure
That might evolve to
Ventilator Dependent Respiratory Failure
That Becomes
Acute Respiratory Distress Syndrome
Clarified as
Community Acquired Pneumonia, secondary to culture positive Staphylococcus Aureus
To identify the problems you need to evaluate the patient’s organ systems in an organized, precise and systematic way. The way I go through the systems is as follows:
NEURO SYSTEM
- •The patient has a “Low GCS secondary to….” traumatic brain injury (specify), stroke, encephalopathy, encephalitis, meningitis, cause uncertain etc.
- •The patient has “Severe Delirium with a RASS score of…..being treated with…..
- •The patient is in “Status Epilepticus being treated with…..with a know or no known history of Epilepsy”
- •The patient has “Guillain Barre Syndrome, requiring mechanical ventilation being treated with plasma exchange”
RESPIRATORY SYSTEM PROBLEMS
Problems with the respiratory system are usually 1. problems with the lung parenchyma (gas exchange) or 2. problems with the airway (particularly airway obstruction)
Parenchymal Problems
- Acute Hypoxic (AHRF) or Hypercarbic Respiratory Failure
- •Ventilator Dependent Acute Hypoxic Respiratory Failure
- •ARDS requiring prone positioning and neuromuscular blockade
- •AHRF requiring high flow or CPAP
- •Acute Hypercarbic Respiratory Failure requiring NIV (BiPAP)
- Airway Problems
- Airway Obstruction requiring NIV
- •Acute Severe Asthma requiring
- •Triggered by……
CARDIOVASCULAR SYSTEM PROBLEMS
- •If the Patient is Hypotensive in ICU requiring therapy specify the cause of Shock
- •Pressor Dependent Septic Shock
- •Pressor &/or Inotrope Dependent Cardiogenic Shock
- •Cardiogenic Shock Requiring Balloon Pump or VAD
- •Pressor Dependent Neurogenic Shock
- •Fluid Responsive Hemorrhagic Shock
Although rhythm disturbances causing hypotension are technically “cardiogenic shock” nobody really uses that term, generally we describe the problem
- •Complete Heart Block requiring external pacing
- •Fast Atrial Fibrillation requiring an amiodarone infusion
- •Runs of Non Sustained Ventricular Tachycardia requiring……
KIDNEY PROBLEMS
- •The patient has “Acute Kidney Injury secondary to (sepsis or rhabdomyolysis or prolonged hypotension) requiring Continuous Kidney Replacement Therapy”
- •You might also qualify this with “on a background of CKD”
- •“Dialysis Dependent AKI – he receives intermittent hemodialysis for 3 hours each day”
- •“AKI no longer requiring Kidney Replacement Therapy”
ENDOCRINE AND ELECTROLYTE PROBLEMS
•Hyponatremia, Hypernatremia
- •Hyperkalemia, Hypokalemia
- •Hypomagnesemia, Hypocalcemia, “Hypophosphatemia requiring 4 hourly replacement”
- •There may be a precise diagnosis “High Output Stoma requiring replacement of several electrolytes”
- •Fluid Overload
GASTROINTESTINAL PROBLEMS
There may be a headline diagnosis such as Pancreatitis, Bleeding Esophageal Varices, Small Bowel Obstruction etc.
- •Gastroparesis
- •Ileus (small or large bowel?)
- •Diarrhea
- •Constipation
- •Malnutrition
NEUROMUSCULAR PROBLEMS
- •Hemiplegia
- •Paraplegia
- •Dysarthria, Dysphagia
- •Bulbar or Occular Palsy
- •Critical Illness Polymyopathy
SKIN AND EXTREMITY PROBLEMS
- •Limb Ischemia
- •Edema – upper limb, lower limb, unilateral, bilateral
- •Skin Rash – local or general
- •Wound Infection or Dehisence
- •Bed Sores
HEMATOLOGICAL PROBLEMS
The patient may have been admitted with a hematology issue e.g. thrombotic thrombocytopenia purpura (TTP) or a complication of chemotherapy or bone marrow transplantation
Otherwise
•Anemia, Polycytemia, Thrombocytopenia
INFECTIOUS PROBLEMS
The infection may be the primary problem or it may be secondary
- •Wound contaminated with VRE or Pseudomonas
- •Patient may have acquired MRSA
- •Patient may be isolated due to CPE
RESOLVED PROBLEMS
- •If the patient was admitted with sepsis – source control may have resolved the problem
- •An underlying cardiac problem may have been fixed by a stent
- •An obstructed bowel or leaking aneurysm may have been surgically repaired.
- •Acute kidney injury may have resolved
- •Is anything ever fully resolved?
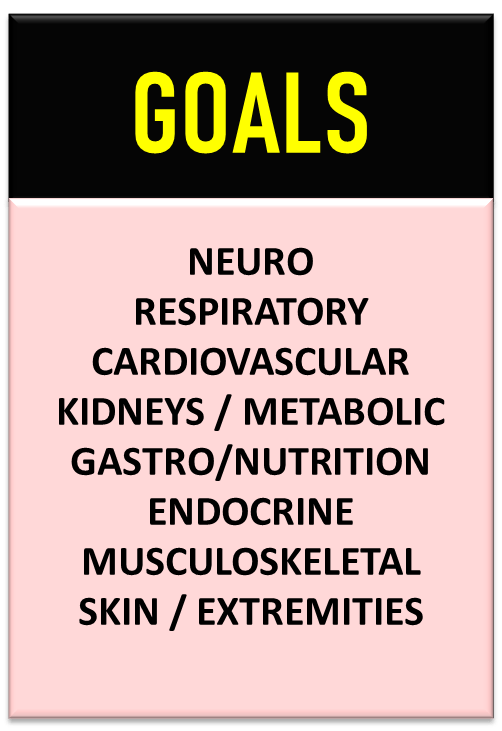
WHERE?
We can’t determine where we are going if we don’t know where we are now! From the outset, the physiological parameters under your control must be targeted: level of sedation, heart rate, Blood pressure, PaO2, PaCO2, pH, urinary output, enteral feeding, fluid balance, mobilization etc.
What physiologic targets have we set for this patient?
- •Neurological – RASS score (or GCS) target with sedation
- •Respiratory – PaO2, SpO2, PaCO2, respiratory rate
- •Cardiovascular – BP (S/D/M), Heart Rate, SV, SVV
- •Gastro/Nutrition – Enteral Feeds, Bowel Motions
- •Renal – Urinary Output, Electrolytes, Fluid Balance,
- •Endocrine – Blood Glucose
- •Extremities – Mobilization
PRESENTING THE CASE
You don’t need notes to present a quick history, summary, problem list and goals of therapy. This should be drawn from memory as often the history is presented several times a day at handovers, rounds etc. Keep the narrative succinct – don’t stray off track – we are interested in the FACTS the FACTS and nothing but the FACTS.
Follow the system in the image below:
This Mr Eddie Chambers he is a 73 year old retired farmer from Mayo
He is a medical patient
He has been in the ICU for 4 Days………having originally been admitted with acute hypercarbic respiratory failure secondary to pneumoni
He was admitted to ICU for intubation and mechanical ventilation
He subsequently developed septic shock and acute kidney injury, requiring pressors and RRT
He has a background history of hypertension treated with calcium channel blockers.
His current problems are: ventilator dependent respiratory failure, pressor dependent septic shock and dialysis dependent acute kidney injury
He is also malnourished, due to gastroparesis, hypoalbuminemic, anemic and has a hyperchloremic metabolic acidosis and stress hyperglycemia
He also has an early sacral pressure sore
Our goals are to:
Sedate to a RASS score of minus 2
Reduce the ventilator settings
Keep the PaO2 above 8kPa (60mmHg)
Keep the PaCO2 between 5.3 and 6kPa (40-45mmHg)
A MAP of 70mmHg
Fluid balance of -1000ml today on Kidney Replacement Therapy
We are starting TPN today, and targeting a
Blood glucose below 10mmol/L (180mg/dl)
Sit him out in a chair today
REVIEW
This Tutorial Looked at Getting a History in the ICU. It is not easy because the patient is usually not able to communicate effectively. Significant detective work may be required.
Who – who the patient is
Why – the patient came to hospital and why they needed to be admitted to ICU
What is currently wrong with the patient (Problems)
Where – what are our GOALS of management
